We sat down with PREG founder and medical director, kDr. John Nichols to talk about the evolution of reproductive endocrinology and fertility treatment.
 Dr. Nichols, please explain how infertility care and treatment have grown since its inception.
Dr. Nichols, please explain how infertility care and treatment have grown since its inception.
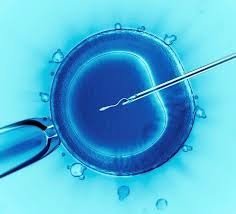
Back in the day when infertility medicine had begun, there weren’t as many options as there are today. For example, if it was a male factor and there were sperm issues a lot of times that’s where donor sperm came into vogue and a lot of patients were using donor sperm for those issues. And, that has all changed because now we can do invitro and IVF where you take a single sperm and inject it into the egg in the lab. This has given these men who years ago would never have any offspring based on their sperm testing. One of the big advantages that have happened over time with IVF is having the ability to treat male factor in a lot of ways that we previously had no choice but donor sperm.
What are some of the advances you’ve seen?
Previously the only other treatment options for most patients were fertility drugs and then intrauterine inseminations. In those days there was a lot of treatment for the fallopian tubal disease. Those are very important for egg and sperm to meet so surgery was indicated for many of those patients. Surgery doesn’t fix a bad tube and the results were pretty poor. This is where in-vitro fertilization began. It was devised for patients with tubal disease who couldn’t get pregnant. So we learned how to extract eggs by bringing them into the lab and fertilizing them with sperm and then putting the embryos back into the patient.
IVF has come a long way and we clearly use it for patients with tubal disease, and we just discussed how it has changed with male factor infertility now that we can go into the testicles and extract sperm and use that sperm to fertilize eggs and we’ve come a long way with that side.
 How about embryology?
How about embryology?
The improvements of what we have done with growing embryos in the lab, cultured media, the lab environment, incubators, and, all of the technology we have been able to improve. It helps us to get the best quality embryos and transfer them back to get the higher pregnancy rates. The discipline has been so strongly impacted by the advent and growth in IVF. It has allowed us to do things for patients we were never able to do before so IVF is clearly the big shining approach in our treatment entree’ to help a lot of patients.
How have donor bank protections and screenings improved over the years?
What is interesting is before HIV came on the scene a lot of sperm donors were fresh donors. A lot of guys would come off the street and they would collect the sample that day and the physician would wash it and process it and put fresh sperm right into a patient if she was using a donor. They had a lot of donors for fresh sperm and fresh sperm is always better than frozen sperm. However, in the late 70s and early 80’s HIV hit and unfortunately a lot of donors were gay men and women were getting infected with HIV positive sperm before we understood what was going on with HIV. The FDA came in and changed all the rules and said no more fresh sperm donors. Today all sperm donors have to be screened for all STDs. If they are positive they will not become a donor.
Today we collect samples and there is testing for all STDs (gonorrhea, syphilis, chlamydia, HIV), Hepatitis B and C, etc. There are essentially three sets of testing anywhere from three to six months apart. Before they release that sperm the donor is retested and if the donor is still negative they will release the sperm. The screening has really improved.
 What about STD screenings for monogamous couples? Do they need it?
What about STD screenings for monogamous couples? Do they need it?
No, because the difference who have been having sex whether married or not, they are ready and resistant to anything that could happen between them. We don’t screen these males. When you are using a donor that is not related to one of the parties then you have to screen for what I just mentioned. There are no rules that you have to test couples who have already been intimate.
The process of using gametes, eggs, sperm from donor banks is really rigorously controlled by the FDA. The FDA can show up any day at your practice and these inspections are always unannounced. They come in one morning, introduce themselves and say they are there to inspect the labs, review your books and paperwork. This has really helped raise the bar in accountability and compliance. The FDA is simply ensuring that practitioners abide by the standard protocols and guidelines. All fertility and IVC centers have to follow the same guidelines. At PREG, compliance is never compromised and we welcome it because we care deeply about our patients and our medical discipline. For us it is about protecting our patients and making sure they don’t get anything they didn’t sign up for and we are always following strict adherence to these guidelines.
What about the growth and advancement of genetic testing?
Once IVF was developed and once we could address some of these problems as we were able to grow embryos in the lab, researchers, physicians and scientists began to discuss the possibility of ways to advance genetic testing and remove cells of serious diseases and conditions. In the last ten years we have come a long way in this area. Now we can test for genetic disorders like Down Syndrome, Turner’s Syndrome and things that can be lethal and cause major problems. We can actually test to prevent diseases such as Sickle-Cell, Cystic Fibrosis, all these different carrier diseases and we can even test the embryo to make sure they are not infected. Genetic testing has come a long way with IVF and all the things we are able to do with embryos. We can identify normal embryos, infected ones with some type of disease and transfer that. We can actually take a couple that has a specific disease and we can stop a disease in its tracks that is genetically transmitted.
We can screen and find uninfected embryos so that automatically stops the transmission of that disease in that specific family line from there on.
 Can you please speak to the bioethics involved here?
Can you please speak to the bioethics involved here?
As far as genetic diseases I think it’s very important because I don’t think anyone wants to sign up to have a child that has severe medical disorders that are lethal and will create a whole series of debilitating medical and financial challenges. When you think of the whole medical field as a rule it makes sense that you wouldn’t want to help a couple experience this and someone go into the healthcare system with a child that would have these types of diseases. The reality is that if we did enough testing we could actually wipe out some of these genetic diseases and they would never come up again. You can stop the disease in its tracks! Some people say, “Well you’re playing God here, testing embryos and picking which ones should go back,” and I get all that but for the good of the patient, offspring and the overall health community it seems like a pretty straightforward thing.
Is this a prime example of the Hippocratic Oath?
“First, do no harm.” And I don’t disagree with that at all. You can have all kinds of people argue different sides of this like the Pro-life side that says we don’t have to do all this the embryo could still be fine and the baby could be a contributor to the world despite having a specific disorder or disease. I’m not going to argue that, but we also know that there are some horrific and terrible outcomes that can be medically and scientifically avoided. It’s a huge burden for the family, patient and the healthcare system. You can be on either side of this thing, but when I look at the big picture of this and the good that can come of it, I think in my mind, I’ve resolved it a long time ago, the good outweighs the bad.
What’s on the horizon in your discipline through research, science and testing?
I think all that is happening with these embryos in the lab and how we can start looking at them and things we can do to give the patient the most optimal outcome. What each patient that comes into our offices wants is obviously a child, but even more importantly they want a healthy child. These are the things that we are able to do now with genetic testing and be able to understand what diseases are caused genetically.
Now when you are looking at some of the newer things where people are talking about gene editing and people go in with CRISPR technology and actually go in and edit some of these things in the embryos and take key bits of what is abnormal and then fix it so it’s normal is the next wave. Now, it’s a ways off, but many of these studies are already being done on animals and China has already started with human testing. Of course it’s a different world in China in regard to regulations, but what I’m leading to is that I perceive probably in 10-18 years this stuff is going to be the norm.
 Let’s be clear, I’m not talking about manipulating the genetic code or construction to produce a 6’3” child, hair color and IQ. I’m not so sure that is so easy to do, but what PREG is looking at is what can we do to make the healthiest embryos and children possible. This is the exciting stuff on the horizon. How to decode and look at the entire human genome has made a huge difference. Every time you turn around you see advances in genetic screening and things like Ancestry.com and other resources that will provide things to correct at the earliest stages. We are a long way from this but I think this is going to be an incredibly viable option for many couples as we help them achieve our goal of one healthy child at a time.
Let’s be clear, I’m not talking about manipulating the genetic code or construction to produce a 6’3” child, hair color and IQ. I’m not so sure that is so easy to do, but what PREG is looking at is what can we do to make the healthiest embryos and children possible. This is the exciting stuff on the horizon. How to decode and look at the entire human genome has made a huge difference. Every time you turn around you see advances in genetic screening and things like Ancestry.com and other resources that will provide things to correct at the earliest stages. We are a long way from this but I think this is going to be an incredibly viable option for many couples as we help them achieve our goal of one healthy child at a time.
Right now these are some of the things we are able to do for our patients. To screen for diseases and disabilities that can be eliminated for those wanting a child. The bottomline is seeking the most favorable outcomes for our patients and helping them grow their family one baby at a time. We are here trying to correct imbalances not enhance abilities and there is a huge difference.
John, you founded PREG, did you ever imagine the growth it would experience?
Now we stretch from Asheville all the way through South Carolina to the Lowcountry in Summerville. We’ve got a huge swath we now cover. We want to bring our expertise and level of care to these areas to help the many patients who struggle with infertility and care. It’s always been our goal to respond to the growing need of our patients and that’s been incredible. In Asheville, we are pulling patients from Tennessee and pulling down to Georgia and along the coast through the Upstate and the Midlands.
There are markets south of Charlotte, north of Atlanta that we could go in and really help patients. Our CEO, Faith Ripley has told me “no more new offices for awhile!” (Chuckle).
John, did you ever dream PREG would grow to this level?
Not at all. Quite honestly, I enjoyed working at the hospital in Greenville, but there was so much red tape and felt it tied my hands as to how I thought a patient should be taken care of in a big system. I just wanted to open a nice, small boutique practice in Greenville and do my thing. I think we put together a very good model to achieve that but a lot of areas throughout the region were like, “Hey, wait! We want those options here.” And so here we are. It’s been an exciting journey. If you had told me years ago that we would have five offices spread across the Carolinas I would have said, “No way!” It’s been quite a ride.
 PREG has IVF Centers Greenville, Columbia and Lowcountry with offices also located in Spartanburg and Asheville. We offer highly personalized fertility care and management. Dr. Nichols is based in the Greenville, SC, office. For more information on reproductive options call, or contact us today at 866.725.7734.
PREG has IVF Centers Greenville, Columbia and Lowcountry with offices also located in Spartanburg and Asheville. We offer highly personalized fertility care and management. Dr. Nichols is based in the Greenville, SC, office. For more information on reproductive options call, or contact us today at 866.725.7734.