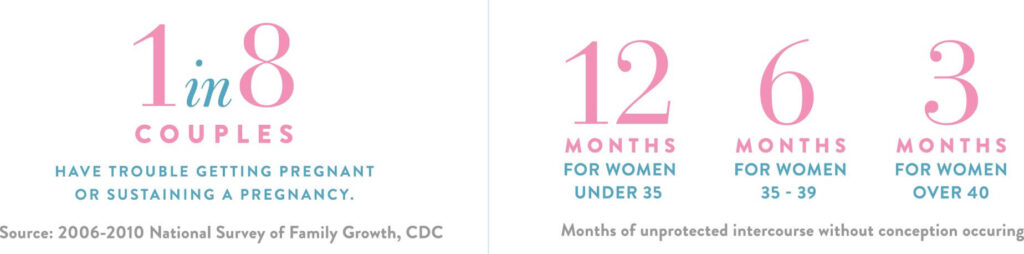
When should I schedule an appointment?
Anovulatory Infertility.
Anovulatory infertility occurs when a woman does not ovulate, meaning her ovaries do not release an egg during the menstrual cycle. Without the release of an egg, fertilization by sperm cannot occur, making pregnancy very difficult to achieve without help. This type of infertility is often caused by hormonal imbalances that disrupt ovulation. For example, a condition called polycystic ovary syndrome (PCOS) can upset the balance of reproductive hormones and prevent regular ovulation. Abnormal thyroid hormone or prolactin (a hormone from the pituitary gland) levels can also interfere with ovulation. Lifestyle factors play a role as well – obesity or, conversely, being underweight can alter hormone levels and interfere with ovulation. Ovulatory problems are one of the most common factors in female infertility and roughly 25–30% of infertility cases in women can be attributed to chronic anovulation.
Male Factor Infertility
The most common causes of male infertility are related to sperm production and function. In a healthy male, the testicles produce millions of sperm cells. However, in some instances the sperm do not develop properly, there are too few sperm being made, or the sperm that are produced may have an abnormal shape or poor motility which impact function. Other causes of male infertility include imbalances of the hormones that regulate sperm production and blockages in the male reproductive tract that prevent sperm from being ejaculated. Additionally, certain lifestyle factors (such as heavy smoking, alcohol or drug use), past infections (like mumps affecting the testicles), or injuries to the reproductive organs can contribute to male infertility.
Our reproductive specialists are fully capable of thorough male evaluation and related counseling. For those with very low sperm production who require surgical sperm retrieval for IVF, the procedure may be performed at our center. We also work closely with local fertility urologists who can coordinate further evaluation and treatment when necessary.
Tubal Factor Infertility
Tubal factor infertility arises when the fallopian tubes are blocked, scarred, or otherwise damaged, which means the sperm cannot reach the egg for fertilization, or a fertilized egg cannot travel down to the uterus. As a result, even if ovulation and sperm production are normal, the egg and sperm are physically prevented from uniting to start a pregnancy. The leading cause of tubal infertility is damage from prior infections such as chlamydia, gonorrhea, or pelvic inflammatory disease (PID) – a serious infection of the reproductive organs. Endometriosis, a condition where tissue that normally lines the uterus grows outside of it (such as on the tubes or ovaries), can also lead to tubal damage. Previous surgeries or ectopic pregnancies (a pregnancy that occurs in a tube) can also lead to scarring in or around the tubes, affecting their function. In some cases, though less common, a woman might be born with an abnormal tube structure.
The most specific test for tubal function is a hysterosalpinogram (HSG), which can be performed at PREG. In some cases, minimally invasive surgical evaluation/treatment may be necessary.
Unexplained Infertility
Unexplained infertility is diagnosed when complete fertility evaluation does not reveal a cause for infertility. In other words, all the test results come back normal – the woman is ovulating, her tubes and uterus look healthy, the man’s sperm count and quality are fine – yet the couple still cannot conceive. We understand that most find this diagnosis frustrating, but it may be helpful to learn that it is common (15-20% of cases of infertility), associated with a number of treatment options, and associated with a favorable likelihood of successful treatment in most cases.
Recurrent Pregnancy Loss.
While many view recurrent pregnancy loss (RPL) and infertility as separate entities, there is a spectrum of reproductive dysfunction and both may represent different manifestations of the same underlying factor in many cases. RPL is defined as three or more miscarriages, even if healthy live birth(s) has been achieved along the way. Evaluation is typically recommended after just two pregnancy losses. RPL is incredibly disheartening for those who experience it, but it is important to understand that the likelihood of ultimately achieving a successful pregnancy is much more favorable than most realize, with or without directed treatment. Our reproductive specialists stand ready to learn more about your history and plan for proper evidence-based evaluation. In many cases, a causative factor is not identified, but effective treatment is still available.
Age and reproduction.
The reproductive aging process clearly impacts the likelihood of achieving pregnancy without treatment, fertility treatment-related prognosis, and the risk of miscarriage. Ovarian reserve is a term reflective of egg number and quality. Specific ovarian reserve tests are indicators of egg quantity while age is the most important determinant of egg quality. Overall interpretation is complex and will be a focus of discussion with your reproductive specialist as results impact counseling regarding treatment options, how they compare, and likelihood of success. For women, the window of peak fertility is limited and fertility starts to slowly decline after the age of 35, and more rapidly after the age of 40 with diminishing egg quantity and quality. For this reason, more, rather than less, efficient/effective/aggressive treatment is typically recommended sooner, rather than later, with advancing age. While male fertility also declines with age, the effect is generally less pronounced than in women.
Other ways we can help.
- Fertility treatment for unpartnered individuals or same-sex couples
- Fertility treatment to avoid transmission of a known genetic disorder
- Third party reproductive treatment (donor egg IVF, donor sperm-based treatment, embryo donation, utilization of a gestational carrier)
- Prior tubal sterilization
- Family gender balancing
- Fertility preservation (elective or prior to cancer treatment)
- Genetic carrier screening, fertility testing, and procreative counseling
- Surgical management of gynecologic conditions with reproductive impact
- Treatment of endometriosis, PCOS, and other reproductive endocrine conditions even when pregnancy isn’t an immediate goal