What is IVF?
In vitro fertilization (IVF) represents the most efficient and effective treatment for all types of infertility and the only option for many. At PREG, we use the most advanced technology and latest research to help you achieve your dream of building a family. Many factors lead to a decision to pursue IVF. Both a comparison to treatment alternatives and reasonable expectations regarding response to IVF treatment/likelihood of success are highly patient-specific. These complex but critical concepts will guide discussions between you and your provider following a detailed review of your history and results of recommended evaluation/testing.
How is IVF Different at PREG?
Three IVF Labs = Convenience + Safety + Excellence
PREG represents the largest network of fertility centers in the region, providing care for patients throughout the Carolinas, and beyond. We’ve designed our practice to feature IVF labs throughout the region, rather than one centralized lab, to maximize safety and convenience for our patients. As such, patients seen at any of our centers can rely on the availability of IVF care close to home with staff they’re familiar with instead of having to drive hours away for critical steps in the IVF process.
All of our IVF labs are fully accredited and state-of-the-art, staffed by a team of experienced embryologists and led by our on-site laboratory director, Dr. Jing Chen. Dr. Chen’s experience and dedication are unsurpassed, and her leadership assures consistency among our labs and exceptional outcomes for our patients at all centers.
Of great importance, it is our view that funneling patients from multiple offices into a single IVF lab would compromise both safety and outcomes due to an overwhelming workload that a single lab could not effectively manage. Work within an IVF lab demands focus, precision, and excellence, and errors are not acceptable. As such, we’re proud of our network of IVF labs designed to achieve optimal safety and outcomes for patients throughout the region.
Individualized, yet consistent.
Your provider is the one that knows you best and most capable of determining an individualized IVF plan. In most cases, a patient’s prior experience or treatment will influence their thoughts and expectations regarding further treatment, important information which will always be considered. At PREG, our providers have the autonomy to create patient-specific treatment plans, every single time.
Prior to IVF, you can expect to achieve a clear understanding of the IVF process and your individualized plan. If additional appointments are necessary to achieve clarity, they can be easily scheduled. Extended embryo culture (growing embryos to the blastocyst stage) is the industry standard in modern day IVF and can be expected at PREG. We have the utmost confidence in our ability to optimally culture embryos, a very important factor in a successful IVF practice and one that patients should expect and deserve. Once in motion, IVF cycles are coordinated by a dedicated, caring, and always reachable team of IVF coordinators.
Clear financial advantage.
Some centers do not accept insurance. We are in-network with all and a preferred provider for most. In addition, we’re a network provider for Progyny, WIN, Maven, ARC and Carrot. Other centers overcharge for services for various reasons. We keep our prices fair and competitive to help make fertility care as accessible as possible and utilize the expertise of our financial advisors to look for every opportunity for cost savings along the way. Our patients can expect to pay less for their IVF medications than had they been prescribed by other centers and have access to no-interest financing through PatientFi®, an opportunity available only to PREG patients. We also have a transparent IVF refund program powered by Univfy® for those without insurance benefits and you can expect to meet with a knowledgeable financial counselor ready to advocate on your behalf starting on the day of your very first appointment at PREG.
Additional IVF options.
IVF should not feature a “one size fits all” approach and you can always expect an individualized approach to treatment. At PREG you can also expect options when it comes to IVF-based treatment.
Preimplantation genetic testing (PGT) is an optional, but powerful, component in the IVF setting. You can expect to learn about its capabilities and limitations so you can decide whether, or not, to include it in your care. Your provider won’t make the decision, you will. See our page on preimplantation genetic testing for more information.
Our Minimal IVF program represents a streamlined approach to the IVF process with a goal of reducing the financial burden associated with IVF. It is a reasonable option for some, but certainly not all, patients and your discussions with your provider will lead to a determination of which IVF option is best for you.
Our embryologists are INVOcell® certified, offering an opportunity for intravaginal culture in select cases (Simply IVF). Other options available at PREG include embryo banking, reciprocal IVF (or co-IVF) for same sex female couples, donor egg IVF for all couples/individuals, utilization of a gestational carrier, and PREG’s embryo donation program. Please visit our LGBTQ and third-party reproduction pages to learn more.

What are the steps of IVF?
Preparing for your IVF cycle.
Once the decision to proceed with IVF has been made, your history and the results of your initial evaluation will allow your physician to plan your individualized treatment protocol. You will be connected with an IVF coordinator who will be your primary point of contact moving forward and work with you in coordinating all aspects of your cycle, adapting it to your own schedule. An opportunity for follow-up financial counseling will also be provided prior to moving forward to ensure clarity and that all questions have been answered.IVF stimulation.
A natural cycle (for those who ovulate regularly) typically produces only one mature egg per month. In an IVF cycle, the goal is to generate as many mature eggs as possible. Reasonable expectations will be discussed prior to the cycle and are based on results of your ovarian reserve evaluation.The IVF stimulation phase takes, on average, 10-14 days to complete. The primary stimulation drug, recombinant FSH (follicle stimulating hormone), is bioidentical to the hormone used by the body to make one follicle (which contains one egg) grow. With more FSH present (via administration), more follicles can grow. IVF stimulation medications are administered via a small needle injection beneath the skin (subcutaneous). For most cycles, two injections will be administered at night throughout the stimulation and, about halfway through, a third drug will begin to be administered daily to prevent early ovulation.
IVF stimulation cycles are coordinated around patients’ periods. For those who do not have regular periods, cycle status assessment via ultrasound and blood tests tell us how best to coordinate the start of stimulation. Birth control pills, estrogen tablets, and other drugs may be used for optimal cycle coordination prior to the start of stimulation.
Most patients feel quite well during the stimulation phase and the number of monitoring appointments necessary is less than most realize. All appointments are scheduled well ahead of time to allow you to adjust your schedule at home or work and are brief. Some bloating towards the end of stimulation is normal and not something that typically interferes with daily life. This phase does fall over a weekend in most of our cycles when, hopefully, you will be able to rest and relax.
The monitoring appointments (typically a total of three) include a blood draw to monitor the reproductive hormones during the cycle and a vaginal ultrasound to carefully track the rate of follicular growth. Once the follicles reach the sizes indicative of optimal development of the overall group, a plan for “trigger” is made, which sets into motion events within the follicle necessary to be able to retrieve eggs from them. The egg retrieval is performed two mornings following the evening of trigger injection.
Egg Retrieval
The egg retrieval procedure is performed under IV sedation. As such, you will be asleep, but not intubated (breathing tube). Licensed anesthesia providers are present at all of our centers for anesthesia administration. Pre-cycle evaluation by our anesthesia team and other medical providers may be necessary for some patients. A BMI < 45 is necessary for IVF at PREG.The procedure is fairly brief, taking around 30 minutes to complete. A vaginal ultrasound is used to guide a needle through the vaginal wall and a very short distance to each ovary. Once the needle is in a follicle the fluid is drained and passed to an embryologist who will identify the egg. One needle puncture per ovary allows access to all follicles.
You will be notified as soon as the procedure is complete how many eggs were retrieved. During egg retrieval sperm is prepared for fertilization of the eggs, which takes place later that day. You will return home following a brief recovery phase. Most patients only require over-the-counter pain medications following retrieval and are able to return to usual activities the next day.
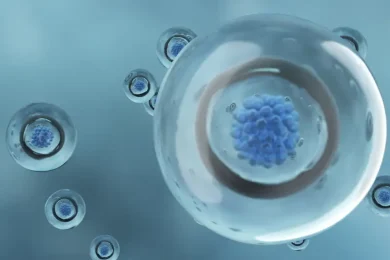
Embryo Culture
Fertilization of the eggs is performed the same day as egg retrieval and can be achieved via either conventional insemination (eggs incubated with sperm) or ICSI (intracytoplasmic sperm injection, where each egg is injected with an individual sperm). The eggs are microscopically assessed the day following retrieval (culture day 1) to determine which fertilized normally and have become day 1 embryos.Extended culture is the standard approach at PREG, whereby embryos are cultured, undisturbed, until culture day 5-6, at which point some, but not all, will have progressed to the blastocyst stage, the stage at which embryos are ready to implant in the uterus with or without IVF. It is important to understand that not all eggs are chromosomally normal, which is why retrieval of as many eggs as possible is important. Embryos which stop developing in culture came from abnormal eggs and would have led to a negative pregnancy test in a natural cycle since they did not progress to the point of implantation potential.
You will be updated by culture day 7 how many embryos progressed to the blastocyst stage. Unless specifically requested by your physician, updates earlier the culture process are not provided as doing so would require removal of the embryos from the culture system/incubator which disrupts steady-state temperature and cell metabolism which may impact developmental potential.
Embryos which become blastocysts may be prepared for embryo transfer (i.e. fresh transfer 5 days following egg retrieval of one embryo with the remainder frozen for future use), biopsied for embryo preimplantation genetic testing (PGT) prior to being frozen, or frozen without biopsy/PGT. The most advanced method of freezing (vitrification) is utilized at PREG.
If not planning for a fresh embryo transfer, plans for subsequent frozen embryo transfer (FET) will be made following the first post-retrieval period or any period thereafter since the implantation potential of embryos does not change with time once embryos have been frozen.
Embryo Transfer
Preparation for embryo transfer and the procedure itself are much simpler and easier than the initial stimulation phase. Coordination is highly flexible and can be easily fit into any schedule. Fewer appointments are necessary during these cycles and patients typically feel quite normal.Estrogen tablets are administered orally (and vaginally in some cases) and an ultrasound performed after approximately two weeks of estrogen administration allows confirmation that the endometrium (uterine lining, where implantation will occur) has proliferated/developed appropriately. At that point, daily progesterone administration begins and the embryo transfer is scheduled a precise number of days later (approximately one week). Embryo transfer cycles can also be coordinated with a natural cycle.
The embryo transfer is a simple, painless procedure that takes only a few minutes to perform. Once a multipoint process with witnessing and verification has been completed to confirm the identities of all parties (patient +/- partner and embryo[s]), your physician will insert a small catheter through the cervix and into the uterus using ultrasound guidance which you will be able to follow along with/see. Once the catheter is in the optimal position within the uterus, the embryo is gently released into the uterine cavity. The procedure is performed with a very full bladder, which makes catheter insertion easier and allows us to visualize the transfer process with ultrasound.
Following embryo transfer your embryologist will microscopically assess the transfer catheter to ensure that the embryo was not retained. At that point, you are free to return to your usual activities. A pregnancy test will be scheduled 10-12 days later and you will continue the same medication regimen started prior to embryo transfer until the 10th week of pregnancy. Any embryos not transferred that day will remain frozen until ready to transfer in the future.