 Tori Bishop MS, FNP-BC, PREG Nurse Practitioner and Director of Nursing, discusses the need for annual fertility testing.
Tori Bishop MS, FNP-BC, PREG Nurse Practitioner and Director of Nursing, discusses the need for annual fertility testing.
Tori, what is annual fertility testing?
Sometimes I think we, as clinicians, do a really poor job of talking to women about taking control of their fertility. It starts in adolescents. We preach don’t get pregnant before you’re ready. Then later, society tells us not to rush a family. Life gets busy and then some women will sit down and they are 45 and want to have a baby, but we start looking at testing and age statistics and there are a lot fewer options because conception chances decline with age.
Women postpone conception for a number of reasons. Some are planning their futures, they are in school, or they are managing busy careers. Whatever the reason, more and more women are having babies later in life. They are also taking control of their fertility when they aren’t ready for a baby in their younger years. Fertility begins to decline around ages 35-38. These women can take control of their fertility through annual testing to help plan for their personal future fertility goals with annual fertility testing.

Not always. I’d like to think of every woman as a forward-thinking caregiver who has this talk every visit, but it just doesn’t always happen that way. Sometimes, you have to request this kind of specific testing at your annual gynecology appointments. In some cases, women’s OBGYN’s or family physicians may tell them at an earlier age that it’s time to consider testing and they need to start thinking ahead in their family planning. Remember this testing is just a good prediction and it isn’t the whole book and it doesn’t write the entire story for you, but it gives you an idea of what your general fertility status looks like. As part of this testing, ovarian reserve testing can be used by patients to decide if they want to cryopreserve or “bank” their eggs to be used in future fertility plans. Remember that fertility planning isn’t just having babies right then but also thinking about storing eggs or embryos for use later in life.
What’s involved in annual testing?
We test to screen for GYN conditions such as ovarian cysts, fibroids, polyps, and endometriosis. These are things that might impact fertility. Addressing or identifying these conditions now can help a patient to conceive later.
Much of it depends on what her overall life goal is in regard to family planning when they want to start trying to conceive. I would definitely recommend starting in your late 20’s or early 30’s at least have a discussion with your gynecologist if you are considering waiting for conception until later. This allows for better planning and more options as younger women typically have better success chances. Some of this testing, including lab work and pelvic ultrasounds, is also the same type of testing we do for egg donors. Some of these younger women who undergo testing may even be excellent candidates for egg donation. But it will help them decide if egg banking for the future is right for them. I would say if you are considering getting pregnant in the not-so-near future, then it’s time to have some of this testing done.
What other testing is done?
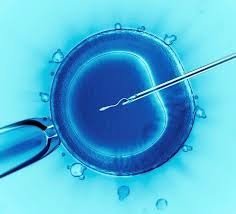
Two main tests that are predictors of fertility and how women will respond to fertility treatments or fertility preservation are their anti-Mullerian hormone or AMH and their antral follicle count or AFC.
It usually starts with an ultrasound. A quick peek at the uterus and ovaries gives so much information. The antral follicle count (AKA the resting egg count) is suggestive of her overall fertility. We will correlate to labwork. While the antral follicle count drops with age there is no real way to predict which patients have a high reserve or how fast they decline. Men are almost always constantly making new sperm but women have a lifetime limit of eggs and are constantly using them up or having age-related changes that occur to them that make them not viable for conception.
Now the AMH or basic hormone testing. An AMH should be roughly in a range of about 1 to 5. The higher the number equivocates to more eggs, so lower numbers, especially less than 1 equals diminished ovarian reserve which limits conceptions options again. Sometimes we draw a few other hormone labs as well depending upon general age, how long until ready to conceive and family history can occasionally play a part in what other labs are drawn. Labs are typically tailored to the individual.
What about women who have previously conceived, but a few years have passed and they are considering conceiving again?
If you are under age 35 and you are having unprotected intercourse for over a year, then it’s time to start looking for help. But also, if you had that first baby at 28, and now you are 33, but not quite ready yet, again it may be a good idea to explore your options through testing because at 35 we could find a decline in ovarian reserve and now you have some age-related changes that come into play. So having some testing may help you consider your many options for infertility care down the road if you need it.
What about women who have had two or more miscarriages and still haven’t conceived?
My heart goes out to these women who have had losses. It’s grief like no other and complicated when you don’t have the answer to why it happens. Recurrent pregnancy loss is typically defined as if you’ve had two or more losses. You should consider recurrent pregnancy loss testing when you fall into this category. Not only do we look at the annual fertility testing measures but we can explore many other causes of recurrent miscarriage and hopefully support future pregnancies. Age can be one of these related issues in recurrent miscarriages. We know there is a decline in fertility or egg quality with age. And then things like endometriosis, fibroids, and smoking affect fertility as well. Women can consider some of the aforementioned testings in regard to future fertility because it’s not just age that affects fertility, and there are things women can do now to prepare for future pregnancies.

I tell patients to keep themselves healthy. Get some daily exercise, maintain decent bodyweight, prevent sexually transmitted infections from happening, seek GYN care when you’re hurting or have changes in your menses, and definitely quit smoking! Medical problems like uncontrolled diabetes and hypertension along with other factors like smoking and obesity can really affect future pregnancy outcomes and change your candidacy for fertility treatments. I’m not saying women can’t have babies or can’t have treatment. I’m just saying that taking control of your health now makes everything easier later on and ultimately gives you better success rates at a healthy pregnancy and live birth.
What about insurance coverage in regard to annual fertility testing?
This is always a tricky question. Insurance may not cover some aspects of fertility testing if your provider is specifically looking for fertility purposes as it depends on whether you have fertility coverage or not. At PREG we work very closely with health insurance providers and with our patients to discover the cost of testing and help with financing options if needed. Unfortunately, insurance typically doesn’t have to cover infertility testing and treatment and planning. The good news is that this testing is not outrageously expensive. It’s usually just simple bloodwork and ultrasound so it’s reasonable to determine if the patient should pursue this now, or there is time to wait.
Please address the importance of age markers in regard to women’s fertility planning and testing.
From age 18-29 there is a 25-30% chance of pregnancy each month. From ages 30-34, it’s about 20%. From 35-39, it’s about 15% and from ages 40 and up it’s really low and the numbers for success drop really fast over a short period of time, while miscarriage rates increase really quickly with it.

So if a woman is 30 and hasn’t been able to conceive naturally within 12 months is it time to consider PREG?
If you are less than 35 and you’ve been trying for a year, you need to see a fertility doctor. At 35-38, you need to come after about six months of trying to conceive. If you are 40+ and thinking of conception options, go ahead and make an appointment so we can discuss options. Talk to your OBGYN but you do not need a referral to see us.




 Tori Bishop MS, FNP-BC, PREG Nurse Practitioner and Director of Nursing, discusses the need for annual fertility testing.
Tori Bishop MS, FNP-BC, PREG Nurse Practitioner and Director of Nursing, discusses the need for annual fertility testing.