In-Vetro Fertilization
IVF FAQ's
 What Goes on in the IVF Lab?
What Goes on in the IVF Lab?
Once your retrieval is completed, other than taking your prescribed medications, there is nothing that you can do to positively affect your outcome. The best thing you can do to produce a healthy pregnancy is to rest and leave the embryo culture to us. Your doctor will need to relay pertinent information to you during your cycle so, please provide a number which you can be reliably reached. In attempts to alleviate your anxiety, we have outlined a day by day description of what we hope to see as your embryos develop.
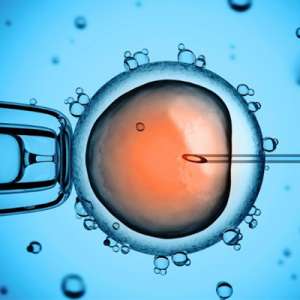
Day 0: Retrieval and Sperm Collection
Following your retrieval your physician will tell you how many oocytes (eggs) were recovered. Not all of the oocytes retrieved will be suitable for ICSI (intra-cytoplasmic sperm injection) or for conventional IVF. ONLY those oocytes that are mature will fertilize. Rule of thumb to remember, anything above 50% is good.
Day 1: 18 Hours Following Retrieval
Woo Hoo! Normal Fertilization has occurred. Fertilization is noted by the presence of 2 pronuclei. This represents the chromosomal material from both you and your husband. Unfortunately at this stage, fertilization is all that we can tell. We cannot accurately predict how the embryos will develop. Once again, a fertilization percentage of over 50% of your mature oocytes is good.
How do Embryos Develop?
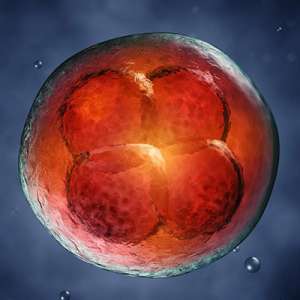
Many factors influence embryo development such as your diagnosis, maternal age, sperm quality, etc. It is not likely all oocytes retrieved will fertilize to become zygotes and not all zygotes will continue to develop into blastocysts. The embryos that develop to the blastocyst stage increase chances of creating pregnancies. Selecting an embryo for transfer on day 5, when zygotes have had sufficient time to develop to the blastocyst stage, helps your embryologist determine which embryo to transfer.
How many Embryos Should I Transfer?
Until recently, it was necessary to transfer multiple embryos to meet this goal. Within the past few years, a rapid increase in the effectiveness of assisted reproductive technologies (especially those which directly affect embryo quality) and a switch from transferring cleavage stage embryos to blastocyst stage embryos has resulted in excellent implantation and pregnancy rates even when only one embryo is transferred. These increases necessitate a switch from transferring multiple embryos to elective single embryo transfers (eSET) – transfers of a single good quality embryo when there are multiple good quality embryos to choose from. eSET is the best way to prevent a high risk and expensive multiple pregnancy. Often patients feel that transferring a single embryo lowers their chance of becoming pregnant to an unacceptable level. However, multiple clinical studies have shown the difference in ongoing pregnancy rates between eSET and transfers with multiple embryos is insignificant. So, while pregnancy rates generally stay the same with eSET, the risk of a dangerous multiple pregnancy decreases substantially. We try to recommend eSET for all of our patients with good quality embryos as a means of providing the best patient care we can.
|
Age |
Recommended # of blastocysts to transfer |
|
< 35 |
1 |
|
35-37 |
1 |
|
37-39 |
1-2 |
|
> 40 |
1-3 |
|
PGS regardless of age |
1 |
How do we decide if an embryo is good quality?
At PREG we remove the embryos from the incubator on Days 5 and 6 to assess quality by looking at them under a microscope. At this time point, embryos need to have developed to the blastocyst stage to be considered for transfer, biopsy and/or freezing.
We look for two distinct cell types in the embryo. One group of cells compacts into a dark spot inside the blastocysts. This group of cells is called the inner cell mass. These cells continue on to eventually form fetal tissue. We’re looking for how tightly these cells are compacted and if there are any cell fragments when determining quality. The other group of cells is called the trophectoderm. They eventually become placental tissue after they implant in the endometrial layer of the uterus. We’re looking for a trophectoderm layer that’s growing in a cobblestone pattern, has a low amount of cell fragments and is composed of many equally sized cells.


 What Goes on in the IVF Lab?
What Goes on in the IVF Lab?